Accreditation for Cardiovascular Excellence recently announced the release of its newly updated, openly available standards for the cardiac catheterization laboratory—standards essential to quality delivery of cardiac Cath/PCI services in all environments.
The update includes brand-new standards crucial to the provision of safe, quality cardiovascular services to patients in Ambulatory Surgery Centers (ASCs), as well as integrating the latest guidance on Cardiogenic Shock (CS) as new standards across all environments.
There are two major areas of update, explains Accreditation for Cardiovascular Excellence's Chief Medical Officer, Bonnie Weiner, MD, MBA. "[The first is] incorporation of a section on the treatment of cardiogenic shock, and the second is a section on ambulatory surgery centers."
This news blog is meant to outline the requirements for ACE’s CathPCI accreditation, as well as the changes to previous editions of the standards, and their concurrent rationales.
What's in this update? Our 2020 standards...
-
…incorporate research and policy that has been generated since our last standards update in 2015,
-
reflect ACE’s internal analyses of standards’ impact on quality at accredited institutions since that time,
-
provide more comprehensive guidance for protocols surrounding cardiogenic shock,
-
and revise & outline requirements for ambulatory surgery centers (ASCs) without access to onsite surgery, as ASCs have recently been accepted by CMS for reimbursement for catheterization procedures.
These changes are part of ACE’s ongoing continual quality update protocols regarding the accreditation process. The goal of ACE’s standards-analysis and the subsequent changes is twofold:
- to ensure that all standards required for accreditation by ACE result in concrete improvements to the care provided by accrediting/accredited institutions,
- and to provide as much flexibility as possible regarding both the expert interpretation of standards, and the ability of facilities with unique resource considerations to seek ACE accreditation.
What’s New for Cardiogenic Shock?
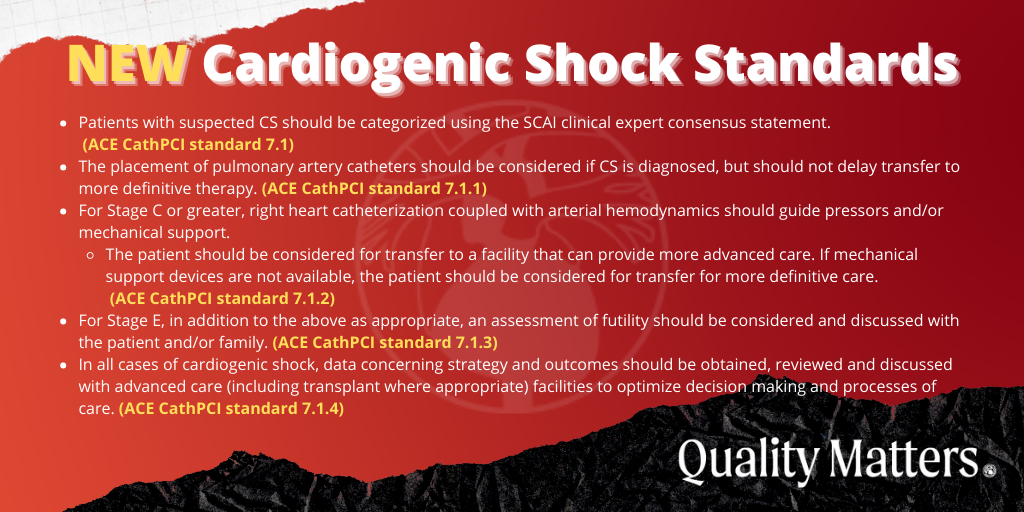
ACE has sought to incorporate recent improvements to our understanding of Cardiogenic Shock etiology and treatment into the standards for CathPCI, understanding that clinical guidelines in this burgeoning area of focus are likely to continue to be a primary concern for cardiology going forward. In the full ACE CathPCI Accreditation Standards document, the following list references standards 7.1 through 7.1.4.
Categorization of CS and subsequent treatment
- Patients with suspected CS should be categorized using the SCAI clinical expert consensus statement. (ACE CathPCI standard 7.1)
- The placement of pulmonary artery catheters should be considered if CS is diagnosed, but should not delay transfer to more definitive therapy. (ACE CathPCI standard 7.1.1)
- For Stage C or greater, right heart catheterization coupled with arterial hemodynamics should guide pressors and/or mechanical support.
- The patient should be considered for transfer to a facility that can provide more advanced care. If mechanical support devices are not available, the patient should be considered for transfer for more definitive care. (ACE CathPCI standard 7.1.2)
- For Stage E, in addition to the above as appropriate, an assessment of futility should be considered and discussed with the patient and/or family. (ACE CathPCI standard 7.1.3)
- In all cases of cardiogenic shock, data concerning strategy and outcomes should be obtained, reviewed and discussed with advanced care (including transplant where appropriate) facilities to optimize decision making and processes of care. (ACE CathPCI standard 7.1.4)
What’s new for Ambulatory Surgery Centers?
In 2010, the passage of the Affordable Care Act required the Secretary of Health and Human Services to outline a plan for value-based purchasing (VBP) reimbursements to go to ambulatory surgery centers (ASCs) under the existing Medicare program. The incorporation of a VBP model for ASC reimbursement demonstrates CMS’s move towards reimbursing based on “value, outcomes, and innovation, instead of merely volume.” Reimbursement focused on value and quality is also expected to improve patient access to procedures, by incentivizing the most efficient delivery of care possible and removing obstacles to care delivery in diverse practice settings.
As clinical proficiency, technological innovation, and the potential for CMS reimbursement in a number of practice settings have expanded over the past decade, the initial impetus for ASC inclusion in Medicare’s VBP reimbursement system – a desire to reward value and quality over volume – has been reinforced, and this trend is expected to continue into the future. As a result, we can safely anticipate that not only will ASCs see increasing volume over the coming years, but also that the quality of care delivered in this unique setting will be held to a high degree of scrutiny.
Accordingly, ACE has expanded our CathPCI Accreditation standards to directly reflect the cardiovascular services and procedures delivered in the somewhat limited environment of ASCs. This was done in an effort to provide straightforward guidance to ASC administrators, clinicians, and support staff in their continuous pursuit of high-quality care and patient safety. Further, by carving out specific requirements for ASCs to achieve ACE’s CathPCI accreditation, we have made it possible for a greater number of healthcare institutions with disparate resources to seek CathPCI accreditation with ACE, demonstrating their commitment to quality care and facilitating their ongoing development as cardiovascular institutions.
ACE’s updated CathPCI Accreditation Standards (which can be viewed here in full), outline several ASC-specific considerations for ACE accreditation in the delivery of catheterization/PCI procedures. An abbreviated list of ASC-specific accreditation standards can be found below. In the full ACE CathPCI Accreditation Standards document, the following list references standards 1.5 – 1.9.8.
ASC licensure, facility, and equipment
- State and federal licensure requirements for PCI providing facilities must be met. (ACE CathPCI standard 1.5.)
- The ASC must have a patient recovery room with at least “semi-permanent, floor-to-ceiling walls,” which is separated from other areas of the ASC and has post-procedure patient monitoring equipment available. (ACE CathPCI standards 1.6, 1.6.1, & 1.6.2)
- The ASC must be equipped with all necessary PCI supplies, including equipment for potentially catastrophic complications. (ACE CathPCI standard 1.7)
ASC capacity, procedures performed, inclusion and exclusion criteria
- ASCs must be capable of performing physiologic lesion assessment with availability of either IVUS or OCT for anatomic lesion and stent assessment. (ACE CathPCI standard 1.8)
- All included and excluded procedures at the ASC must be described and documented. The ASC must be able to easily convert a patient to overnight observation for any same-day surgery PCI procedures. ASC’s must be able to provide confirmation that patients have transport home, social support, and follow-up care. (ACE CathPCI standard 1.9, 1.9.1, & 1.9.1.1)
- These standards indicate that not all hospital same-day surgery patients should be considered for treatment in an ASC.
- This standard reinforces the need for ASC’s to have documented working relationships with full service centers to ensure that patients can be converted to overnight observation when necessary.
- Diagnostic pediatric procedures, procedures for complex congenital heart disease, and pulmonary edema due to ischemia procedures should be excluded from ASC service offerings (ACE CathPCI standard 1.9.2)
- At least 90% of PCI procedures should meet inclusion/exclusion criteria, as demonstrated by internal audit (ACE CathPCI standard 1.9.4)
- Therapeutic procedures for pediatric and adult congenital heart disease should be excluded, and elective and primary PCI procedures are permitted ASCs if there is strict adherence to national guidelines and a documented working relationship with a full service facility, including a tested emergency transport system in place. Elective high-risk patients and high-risk lesions are also unsuitable for care at an ASC. (ACE CathPCI standard 1.9.3)
ASC quality metrics and procedural volume
- ASCs should perform at least 400 diagnostic coronary angiograms and 200 PCI annually, with documented satisfactory outcomes as reported to ACC NCDR, reporting all findings in the registry below the 50th
- Alternate volume minimums considered upon review of quality metrics (ACE CathPCI standard 1.9.5 & 1.9.5.1)
- The ASC should be able to demonstrate a working relationship between interventional cardiologists & cardiac surgery or interventional service at a receiving hospital, including a letter of support to accept cases
- This includes a mechanism for cardiac surgeon or receiving interventionalist to review coronary angiograms before elective procedure & provide comments; surgical backup & interventional support; confirmed availability of cardiac surgery and next available OR prior to elective procedures; a mechanism for direct discussion between the cardiologist and interventionalist or cardiac surgeon in case of urgent transfer; and a written agreement from both facilities including a rehearsed plan for the transport of patients to a full service facility and the ability to have patients on cardiopulmonary bypass or in the receiving catheterization laboratory within 90 minutes of the onset of the emergency.
- The transport provider should be available to begin transfer within 20 minutes.
- A consent form including ownership information for full service facility and/or other ASCs and hospitals should be made available to the patient.
- A documentation of a review of all transferred patients and submission of data to relevant registries is required (ACE CathPCI standard 1.9.6)
- An external audit is required for any ASC with procedure mortality or need for same day emergency CABG in the lowest quartile for two consecutive quarters (ACE CathPCI standard 1.9.7)
- All ACE accredited ASCs should pursue a radial-first approach for PCI. (ACE CathPCI standard 1.9.8)
The standards above, which are pertinent to ASCs, are critical to ensure that quality care can be delivered in the limited ambulatory surgical center environment, and consistently measured. While some are flexible standards (i.e. the procedural volume requirements, and the institution/ASC-specific plans regarding patient transport in the case of urgent transfer to a full-service facility), other standards are more “black and white” (i.e. the prohibition of diagnostic pediatric procedures in the ASC).
About Accreditation for Cardiovascular Excellence
The purpose of accreditation is to ensure quality goals are being met while avoiding prescriptive methods, which risk conflict within existing organizational cultures, understandings, and processes that have been developed through research and practice experience. ACE’s standards that are paraphrased above are designed to set expectations, guide organizational processes, and define clear quality benchmarks for institutions seeking accreditation in CathPCI procedures.
The updated ACE standards represent a “living document” in healthcare. By this, we mean that they are designed to reflect and guide the “moment of decision,” and as such must be flexible enough to account for multiple contingencies, circumstances, and outcomes. Their interpretive nature is indeed a marker of their usefulness as a clinical document. That said, they are not arbitrary, as they reflect the most recent research, scientific consensus, and clinical guidelines. When combined with expert guidance, interpretation, and experience, these standards provide the opportunity to improve care through collaboration – between organizations and ACE, within organizations, and between care providers and patients.
 Accreditation for Cardiovascular Excellence is an independent, physician-led organization that evaluates and monitors facilities providing cardiovascular care. Accreditation awarded by ACE means that the highest quality standards for cardiovascular and endovascular care are met by doctors and staff caring for patients undergoing diagnostic and interventional catheterization procedures.
Accreditation for Cardiovascular Excellence is an independent, physician-led organization that evaluates and monitors facilities providing cardiovascular care. Accreditation awarded by ACE means that the highest quality standards for cardiovascular and endovascular care are met by doctors and staff caring for patients undergoing diagnostic and interventional catheterization procedures.
Learn more about ACE's 2020 standards for Cath/PCI, here.
Contact: Peggy McElgunn, Esq.
Accreditation for Cardiovascular Excellence
Phone: 202.657.6859
Email: peggy@cvexcel.org